Behavioral interventions targeting vaccine adoption, which we designed for a Louisiana health system, have implications for any behavioral intervention aimed at improving and sustaining health behaviors. I recently had the opportunity to share the lessons we learned at a meeting of the Virginia chapter of HIMSS.
Vaccination Rates in Louisiana
Back in early April, a very faint downward slope on new COVID cases was occurring in Louisiana, yet only 27.9% of the population had at least one dose of the COVID vaccine. Another 30-43% said at the time that they would refuse the vaccine. The state was turning down vaccine doses because the demand just wasn’t there. COVID vaccinations were widely available, yet in Louisiana, vaccination rates remained persistently lower than the rest of the US.
Lirio launched a digital health solution in this environment. We partnered with a Louisiana healthcare system to vaccinate their employee and patient population against COVID.
As a social psychologist, I firmly believe behavior is a function of the person and the environment, and the digital intervention we designed reflects that understanding. We defined a comprehensive set of barriers, both the results of the person and the environment, and designed a digital intervention to overcome them.
More than 40 Barriers to Vaccination
We identified a range of more than 40 cognitive and affective barriers, such as:
- Concern about vaccine cost
- Religious beliefs
- Believing in COVID-19 conspiracies
- Believing immunity from COVID-19 is better than immunity from the vaccine
- Fear of needles
- Fears the vaccine will not be as efficacious
- Social norms
With barriers identified, our behavioral designers and creatives developed more than 700 unique digital behavioral interventions to overcome these barriers.
How Our Intervention Works
At Lirio, we start with an understanding of the target behavior – getting vaccinated for COVID-19 – the people we are trying to move, and the barriers that get in their way.
We use behavioral design to create digital health intervention content elements that are infused with behavioral science to overcome those barriers and to amplify the benefits of the behavior we are trying to motivate.
We use an artificial intelligence platform to assemble those content elements into hundreds of unique message combinations so there is a message that’s right for everyone—no matter their circumstance.
Next, our deep learning agent matches those messages to the people most likely to respond and continually optimizes them to achieve improved fit. We have sent more than 2.2 million messages encouraging COVID-19 vaccination.
Deploying the Intervention
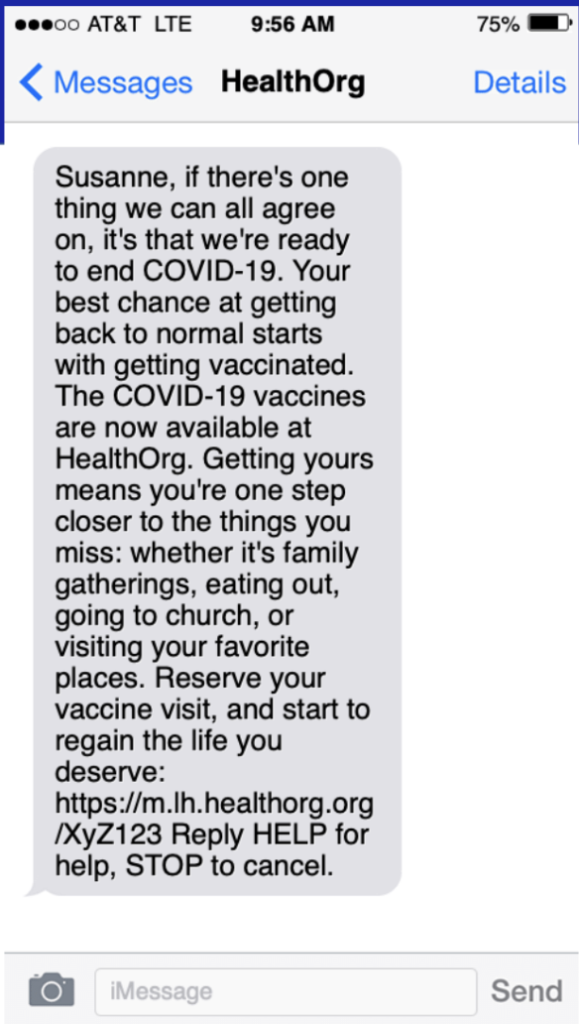
We delivered our interventions via email and SMS. This is an actual message we sent. The message shown leverages incentive – speaking to those things which at the time seemed impossibly far away for many people. We reached over half a million people with our emails and messages.
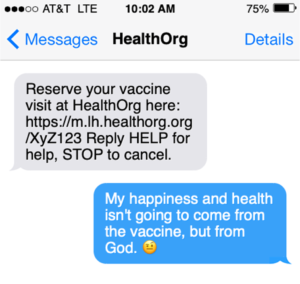
Ten thousand of them wrote us back. These examples are ACTUAL SMS replies to our COVID-19 vaccination digital health intervention. We read every single one of them. In them you see evident many of the known, but also the lesser known, barriers to vaccination. Some barriers we do not address directly, like religious convictions of determinism .
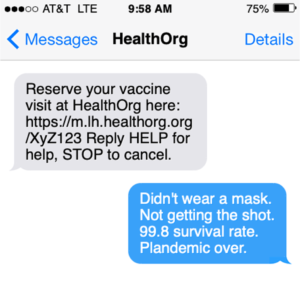
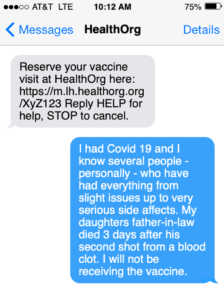
Others we addressed more successfully, such as providing credible and factual information about the safety and efficacy of the vaccine. While there were a number of highly charged message replies regarding our use of the words “safe” and “effective,” we believe strongly in the science behind those statements, so even when we reviewed our content after a few months as things changed with regards to mask mandates and “getting back to normal”, we decided to keep what was, to some, provocative language.
Key Takeaways
The desired behavior was scheduling the COVID-19 vaccine appointment. In addition to patient reactions to our intervention, we noted that different behavioral interventions motivated the four different behaviors of the vaccination journey:
- Scheduling
- No-show to a COVID-19 vaccine appointment
- Obtaining dose 1
- Obtaining dose 2
“When tracking no-shows, we found behavioral interventions like this image—which leverages incentive—to be impactful. The more we leveraged incentive, the less people no-showed.
Scheduling
To motivate scheduling, we mapped messages around incentives. Among people who engaged with messages (n = 5,635), viewing a message with Capability or Opportunity ingredients was associated with keeping scheduled appointments. More specifically, messages with “demonstration of the behavior,” “information about social and environmental consequences,” “information on others’ approval,” “pros/cons,” or “status quo bias” was associated with completing scheduled appointments.
Obtaining Dose 1
Behavioral interventions like this image, which leverages social comparison, was found to associate strongly with obtaining the first COVID-19 vaccine dose.

Viewing a message with Capability ingredients was strongly associated with becoming partially vaccinated. Specifically, messages with ‘demonstration of the behavior,’ ‘incentive,’ ‘information about social and environmental consequences,’ ‘pros/cons,’ or ‘social comparison’ were strongly associated with becoming partially vaccinated.
Obtaining Dose 2
Behavioral interventions like this image, which leverages identification of self as a role model, was found to associate strongly with obtaining the second COVID-19 vaccine dose. In addition, messages with Opportunity and Motivation ingredients were strongly associated with becoming fully vaccinated. Specifically, messages with ‘future orientation,’ ‘incompatible beliefs,’ ‘identification of self as role model,’ and/or ‘social reward’ were strongly associated with becoming fully vaccinated.

The Person, The Context and Timing of Interventions
Getting the first and second dose of a vaccine series are two behaviors more different than we thought. This insight has implications beyond the obvious next behavior: getting the booster and beyond, as well as other vaccination series campaigns like HPV, varicella (shingles), and many childhood vaccines.
COVID-19 is obviously an extreme example of how context shapes — positively and negatively — health behavior. What we’ve learned applies to other digital health interventions as well, specifically within Lirio’s offerings: obtaining mammograms, colonoscopies, attending PCP visits for diabetes control, etc. Each behavior in a patient’s journey should be considered unique, and we can’t take for granted that just because we’ve motivated the first behavior, the rest will follow like dominoes.
We also learned that not only is context important, but timing. Some of our messages fell flat in part because of poor timing. Example: at one point, we were talking about getting back to normal. Then the delta variant began to surge. We were often told—in very colorful language — to get off people’s phones. We now have a better understanding of how people make decisions, based on their own personal characteristics but also on the context and the timing of the intervention.
Addressing vaccine hesitancy taught us a lot about the power of nudging people to better health. To borrow from economist Richard Thaler, “You cannot solve every problem with a nudge, but you cannot solve any problem without them.” We at Lirio are encouraged by the success of this program, and we’re ready to apply lessons learned to future engagements with health systems and payers across the country.
To learn more about Lirio, and to hear from Forrester senior analyst Natalie Schibell about healthcare’s challenges and opportunities in 2022, check out this recent webinar: 2022: The Opportunities of Digitization, the Challenges of Health Equity, Workforce Shortages and Trust.
Others readers viewed:
Lirio Launches Precision Nudging™ Solution to Improve Colorectal Cancer (CRC) Screening Adherence
Lirio Launches Precision Nudging™ Solution for Well Visit Adherence
Lirio Launches Precision Nudging™ Solution to Close Gaps in Diabetes Care
Lirio Launches Hyper-Personalized Vaccination Journey to Encourage Vaccine Acceptance
